2011 study
Laura K. Fonken, Randy J. Nelson
Department of Neuroscience and The Institute for Behavioral Medicine Research, The Ohio State University
Technological advances, while providing many benefits, often create circumstances that differ from the conditions in which we evolved. With the wide-spread adoption of electrical lighting during the 20thcentury, humans became exposed to bright and unnatural light at night for the first time in their evolutionary history. Electrical lighting has led to the wide-scale practice of 24-hour shift-work and has meant that what were once just “daytime” activities now run throughout the night; in many ways Western society now functions on a 24-hour schedule. Recent research suggests that this gain in freedom to function throughout the night may also come with significant repercussions. Disruption of our naturally evolved light and dark cycles can result in a wide range of physiological and behavioral changes with potentially serious medical implications. In this article we will discuss several mechanisms through which light at night may exert its effects on cancer, mood, and obesity, as well as potential ways to ameliorate the impact of light at night.
At different times during our respective childhoods, we both toured Carlsbad Caverns in New Mexico. As part of the tour, the lights in the cave were turned off. The darkness was incredible, engulfing absolutely everything. In our society, we rarely experience such profound darkness; every night, our homes, work places, and streets are brightly illuminated by the glow of electric lights. We will of course always be naturally illuminated by the stars and the moon on a clear night, but we can safely say that most of the light we experience at night is unnatural.
Humans are diurnal, that is, we evolved to be active during the day and to sleep at night. As such, we never developed the ability to see well in the dark. Over time, we have, however, developed the desire to do more and more during the time we are awake, be it night or day, and so we have created an environment that corrects for our relative night blindness. Since the advent of electrical lighting around the turn of the 20thcentury, humans have become increasingly exposed to bright and unnatural light at night. Urban development has further exacerbated the issue, with lighting from infrastructure straying into the atmosphere nightly (). Today, 99% of the population in the United States and Europe, and 62% of the world’s remaining population, are exposed to this “light pollution” [1]. There is no denying that the invention of electrical lighting was a boon for developing industry and technology, allowing the extension of the workday into the night and boosting economic development. However, the use of light at night continues to rapidly increase (by 6% per year) [1] without thorough (or any) consideration of its biological implications.
.
.
.
A common risk factor in many of the pathologies associated with exposure to light at night is a change in immune function, notably inflammatory responses, and recent research has demonstrated that light at night may detrimentally affect the immune system [18]. Thus, in addition to investigating the influence of melatonin and circadian disruption as mechanisms contributing to the maladaptive affects of light at night, characterization of the inflammatory response is also warranted.
One important population that is often neglected when considering light at night is patients in hospitals. While multiple epidemiological studies have been conducted on nurses, there are no studies on the impact of light at night on the patients with whom they work. Many in-patients are already at high risk of increased inflammation and disrupted physiology, which may be exacerbated by light at night.
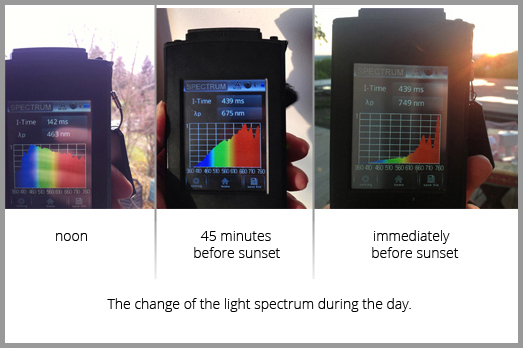
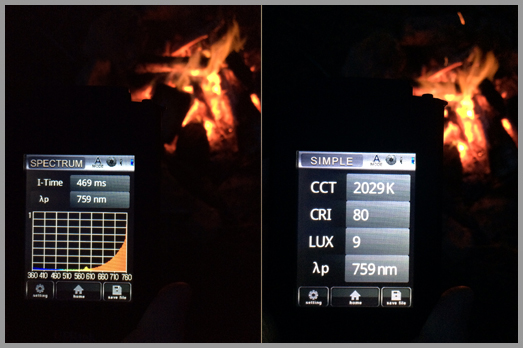
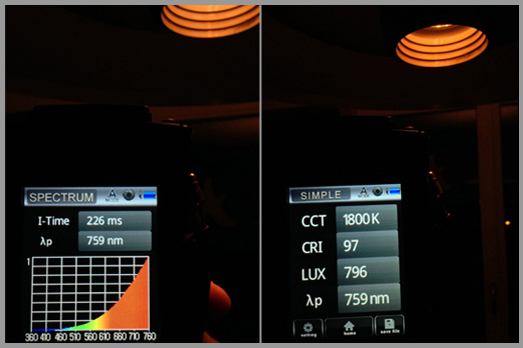
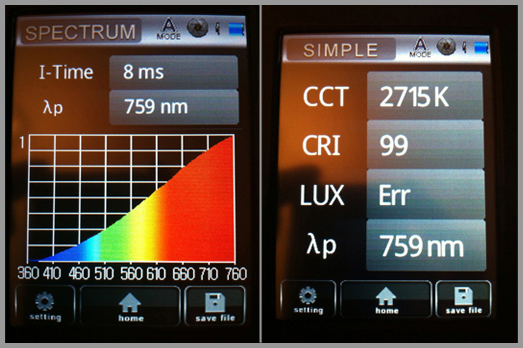
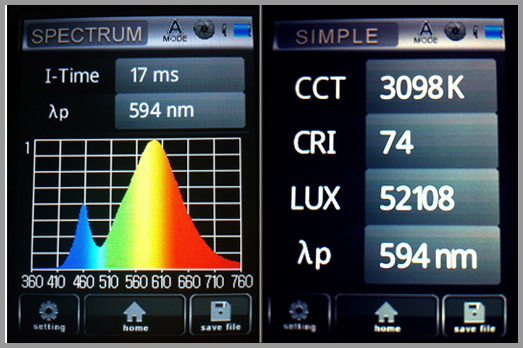
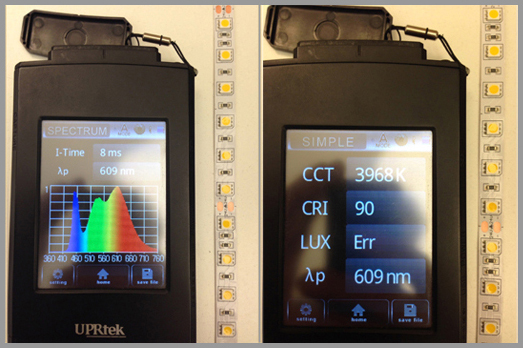
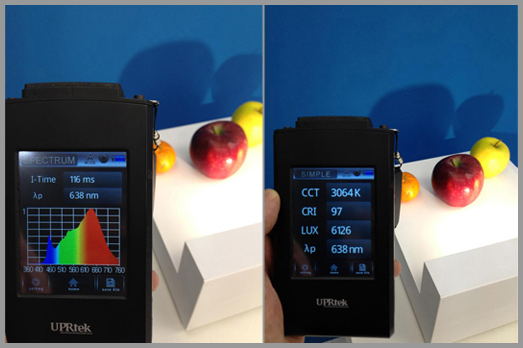
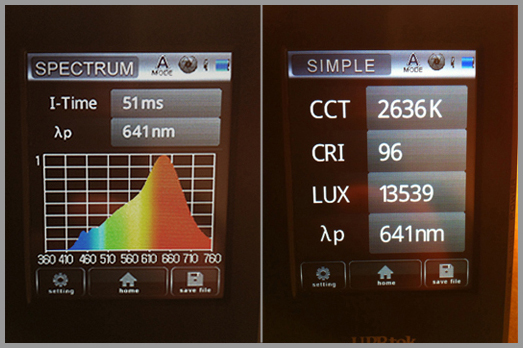
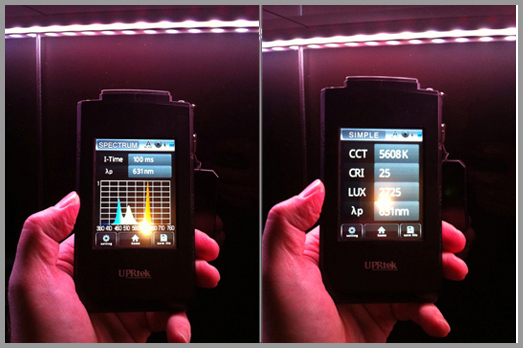
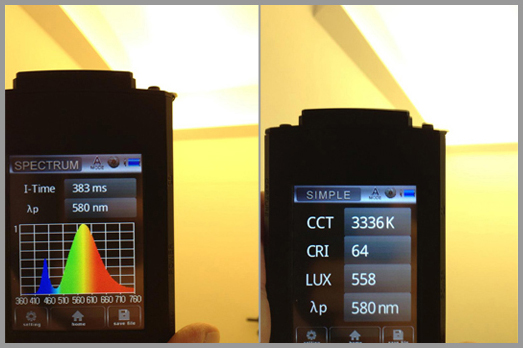
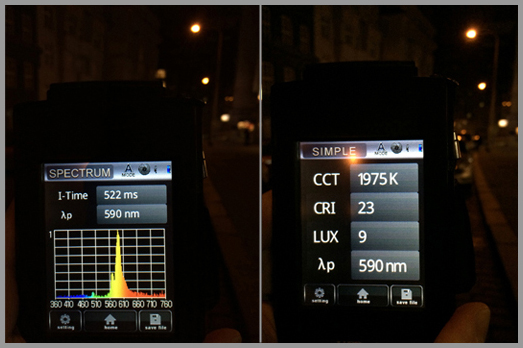
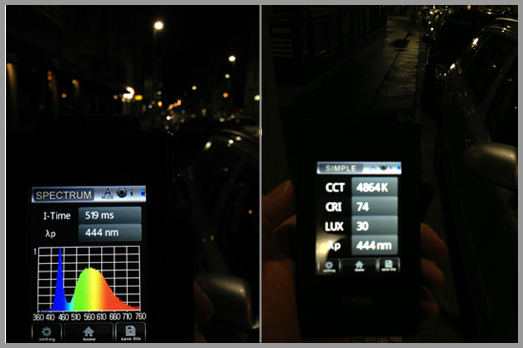
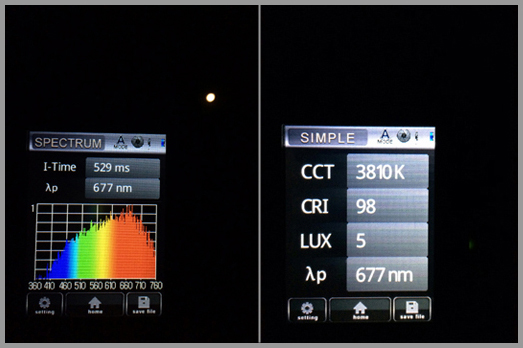
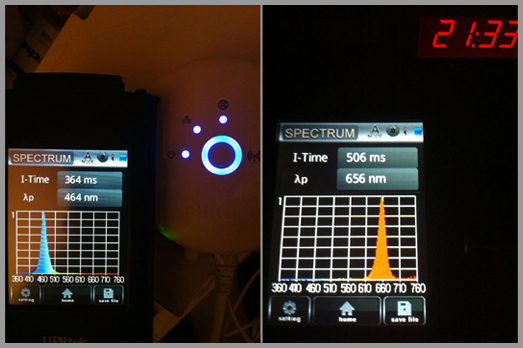
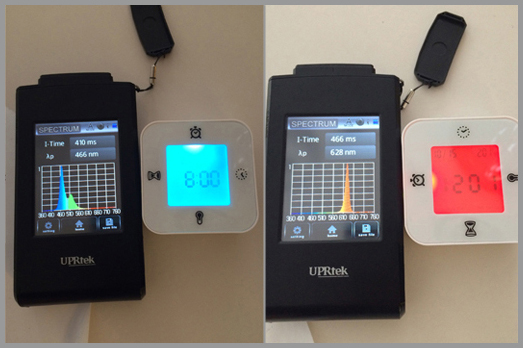
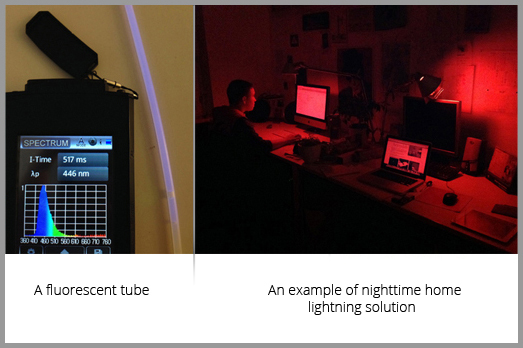
Preventing the general population from excessive exposure to light at night can be achieved with relatively low-cost manipulations, such as using curtains to block out street lights, turning off hallway lights, and removing all light sources, including televisions and computers, from bedrooms. However, these methods do not prevent the extension of daytime hours that many of us experience, but by no means do we recommend that everyone go to bed at sunset. Rather, it may be important for people to try to keep a consistent schedule and avoid rapid shifts in their waking hours. This is often unavoidable in shift-working populations, and there are ongoing studies currently comparing visual aids that may alleviate some of the maladaptive effects of exposure to light at night in shift workers. More specifically, not all lighting has an equal effect; the intrinsically photosensitive retinal ganglion cells that project to the master circadian clock in the brain contain melanopsin and are most responsive to the blue region of the visible spectrum (ranging from 450 to 485 nm), with longer wavelengths of lighting minimally impacting the circadian system. Manipulation of wavelength may prove effective in blocking out some of the light-induced physiological changes. Current research investigating the effectiveness of goggles designed to block out blue wavelength lighting on preventing light-induced melatonin suppression is ongoing. Furthermore, work environments could potentially use lighting sources that emit less blue light, which unfortunately is at odds with the push for energy-saving compact fluorescent bulbs.
Modern society now functions on a 24-hour schedule. Although there are many economic and other societal benefits to such a schedule, there is converging evidence from epidemiological and experimental work that light at night has unintended, maladaptive consequences. In many ways, this field of study is just beginning; further characterization of the impact of light at night is needed along with effective interventions to ameliorate the unintended negative effects of light at night on health.
The entire study, the effect of exposure to light at night can be read at this link.